Emergency Care Newsroom
The Emergency Care Newsroom is your source for industry news, clinical information, product and business updates, inspiring stories and more.

AED buying guide
Approximately 350,000 cases of sudden cardiac arrest (SCA) occur outside of the hospital each year in the United States.1 AEDs are lightweight, portable devices designed to help save people experiencing SCA in public and can be used on children, teens and adults. Even minimally trained bystanders can easily operate them by following audible and visual instructions during an emergency.
Read More
From youth leagues to pros: AEDs play a vital role in safeguarding athletes of all ages
In the fast-paced world of sports, where victories and challenges unfold on the field, athletes face a silent and unpredictable adversary—sudden cardiac arrest. This life-threatening condition knows no age or athletic level, impacting young individuals engaged in youth sports to professionals performing at their peak.
Read More
Sudden cardiac arrest: It can happen to anyone
Derrick Mosley survived a sudden cardiac arrest thanks to his wife's quick thinking and a team of first responders.
Read More
Knowing when to use an AED: CPR and AED guidelines for sudden cardiac arrest
Sudden cardiac arrest is a life-threatening condition that can strike anyone, anywhere, at any time. Cardiopulmonary resuscitation (CPR) combined with the use of an automated external defibrillator (AED) can significantly increase the chances of survival.
Read More
Understanding the basics of a LUCAS chest compression system
Read More
Survivor: Denis Legault
Quick action (and speedy driving) by paramedics helped save sudden cardiac arrest survivor Denis Legault. Two years after the event, Denis met the crew that helped save his life.
Read More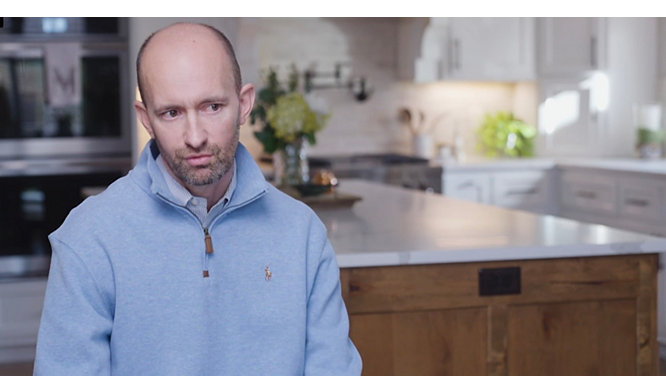
Survivor: Derrick Mosley
After going on a morning run, Derrick began to feel some chest discomfort. His wife, Melissa, a healthcare professional trained in resuscitation, quickly recognized the warning signs of a sudden cardiac arrest. Luckily, an off-duty firefighter pulled over from traffic and began assisting. Soon EMS and Fire/Rescue units arrived to apply a LUCAS.
Read More
Four reasons every school needs AEDs
Read More
How the right equipment can help recruit and retain EMTs and paramedics
Read More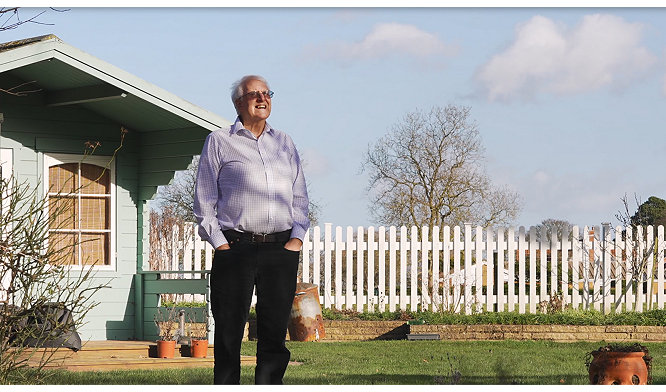
Survivor: Bob Whetton
Seven cardiac arrest events, seven saves. Watch this video to discover more about the cardiac arrest response system at Brighton FC's AMEX stadium.
Read More
Survivor: Andy Hannan
Andy Hannan was playing walking football when he collapsed on the field from a sudden cardiac arrest. Thankfully, one of his co-players, Sue, a first aid volunteer, immediately sprang to action. Watch how she saved his life with the help of the system of care.
Read More
Why every college campus needs accessible AEDs
Automated external defibrillators are an essential part of every college health and safety program
Read More
Survivor: Esley Thorton
The most important thing to Esley Thorton is his family. Watch how they each played a role in saving his life with the help of an AED they keep in their kitchen pantry.
Read More
How to prepare your workplace for a sudden cardiac emergency
Read More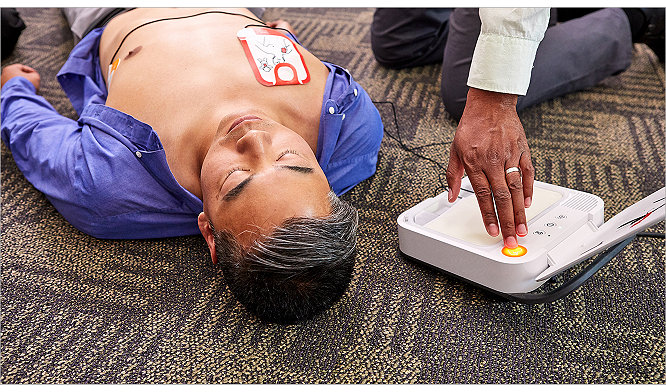
Help increase patient outcomes both in and out of the hospital
Read More
EMS Stories: Provo Fire and Rescue
We spoke with Provo Fire & Rescue, in Provo, Utah. Hear about the care they administer in the back of their ambulance on a day-to-day basis.
Read More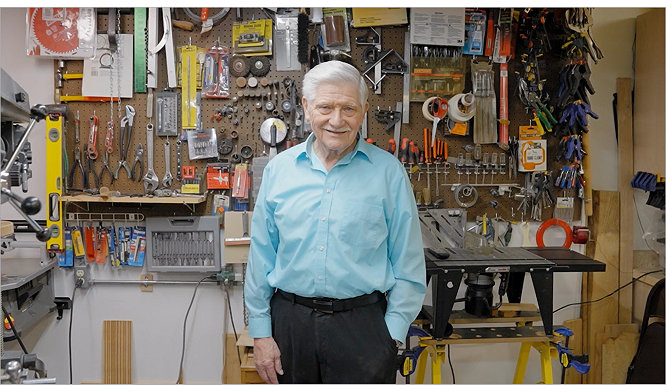
Survivor: Garry Vandenberg
Garry Vandenberg was performing a hymn sing during a church performance when he collapsed on stage from a sudden cardiac arrest. Thankfully, a few key audience members immediately sprang to action. Watch how Stryker’s system of care saved his life and learn how the Kalamazoo community works together to help save lives.
Read More
EMS Stories: Memphis Fire Department
We sat down with the Memphis Fire Department. Hear their perspectives on what it's like to work in emergency medical services.
Read More
The role of defibrillation during sudden cardiac arrest
Read More
Survivor: Bennett Hart
A rare genetic condition caused Bennett Hart’s heart to stop three times between the ages of 8 and 15. Watch how this determined student athlete overcomes every obstacle with the support of his friends and family.
Read More
AED buying guide
Make the right choice when purchasing an AED. Explore the 5 standards to follow and consider Stryker's diverse options for your workplace's safety program.
Read More
Survivor: Bob Zollner
Bob Zollner, a retired firefighter, suffered a sudden cardiac arrest on his wife’s birthday. Watch how she saved his life with the help of their local fire department.
Read More
8 steps to a successful AED safety program
Read More
EMS Stories: Anchorage Area Wide EMS
We connected with the men and women of Anchorage Area-wide EMS for the latest installment of our EMS Stories series. Hear their perspectives on what it's like to work in Emergency Medical Services in the unforgiving, rugged terrain of Alaska.
Read More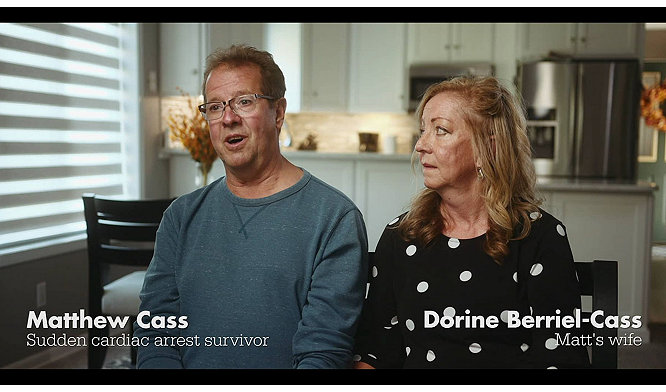
Survivor: Matt Cass
A normal routine changed direction when Matt Cass collapsed from a sudden cardiac arrest during his morning walk. Miraculously, after 80 minutes of continuous CPR and critical care, Matt regained his pulse and started breathing. Listen to his story.
Read More
12-year-old girl experiences cardiac arrest, Stryker employee responds
Read More
EMS Stories: Rescue on Mount Marmolada
As two experienced rock climbers scaled the vertical wall of Marmolada – the highest mountain of the Italian Dolomites – they knew something was amiss when the temperature dropped suddenly.
Read More
Survivor: Jordan Schoen
Jordan Schoen was only 17 when he collapsed on the basketball court. Watch to learn how the system of care saved his life and why this experience drove his family to give back to their community.
Read More
Defibrillator 101
Read More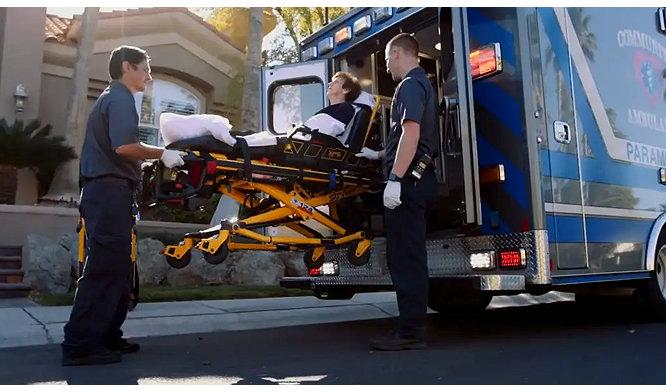
EMS Stories: Community Ambulance Las Vegas
We sat down with the men and women of Community Ambulance in Las Vegas. Hear their perspectives on what it's like to work in emergency medical services.
Read More
5 steps to convince decision makers to adopt an AED program
Read More
EMS Stories: Liverpool P.A.
We follow the volunteer men and women of Liverpool EMS in Liverpool, P.A. Learn how this small town community serves and protects their neighbors every day!
Read More
Survivor: Roger Hildwein
What started out as a productive workout turned critical after our own Staff Mechanical Engineer Roger Hildwein suffered a sudden cardiac arrest in our onsite gym.
Read More

3 ways AED remote monitoring makes a difference
Read More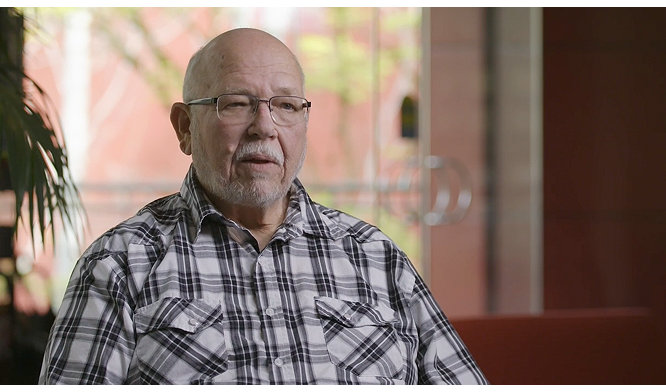
Survivor: Rick Ahrens
When one of our own Team Members, Rick Ahrens, succumbed to cardiac arrest, his co-workers didn't hesitate to start CPR and apply an AED. This is his story.
Read More
Survivor: Bill Krueger
Former Major League Baseball player, William "Bill" Krueger, shares his sudden cardiac arrest survival story.
Read MoreFollow us on social media for more updates:
Celebrate survivors of sudden cardiac arrest
